Cosmetic & Functional Gynecology
Vulval Warts Removal
Vulval warts, caused by certain strains of the human papillomavirus (HPV), are benign growths that appear on the external female genitalia. While they are non-cancerous, they can cause discomfort, itching, and emotional distress. Removal of vulval warts aims to alleviate symptoms, reduce the risk of transmission, and improve the aesthetic appearance of the vulval area.

What to Expect
Before the Procedure: A thorough consultation will be conducted to assess your medical history, examine the warts, and discuss the most suitable treatment options. Preoperative instructions may include avoiding certain medications and arranging for post-treatment support.
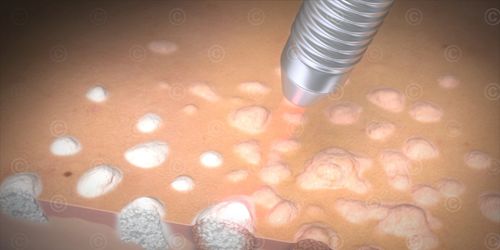
During the Procedure: Treatment options vary based on the size, number, and location of the warts. Common methods include:
- Topical Treatments: Prescription creams like imiquimod or podophyllotoxin applied directly to the warts.
- Cryotherapy: Freezing the warts with liquid nitrogen, causing them to fall off.
- Electrocautery: Burning off warts using an electric current.
- Laser Therapy: Using focused light to destroy wart tissue.
- Surgical Excision: Physically cutting out the warts under local anesthesia.
After the Procedure: Patients may experience mild discomfort, swelling, or redness. Recovery time varies depending on the treatment method, but most individuals can resume normal activities within a few days to a week.
Benefits
- Relief from physical discomfort and itching.
- Reduced risk of HPV transmission to partners.
- Improved aesthetic appearance of the vulval area.
- Enhanced self-confidence and emotional well-being.
- Prevention of potential complications associated with untreated warts.
Ideal Candidates
Vulval warts removal is suitable for women who:
- Have visible warts causing discomfort or emotional distress.
- Seek to reduce the risk of transmitting HPV to sexual partners.
- Desire an improved aesthetic appearance of the vulval area.
- Are in good general health and have realistic expectations.
Pre- and Post-Procedure Care
Preoperative Care: Follow your healthcare provider's instructions, which may include stopping certain medications and avoiding sexual activity before treatment.
Postoperative Care: Maintain hygiene in the treated area, avoid sexual activity until healing is complete, and attend all follow-up appointments to monitor recovery.
Testimonials
"I was embarrassed and uncomfortable due to vulval warts. Dr. Rainee Agrawal provided compassionate care, and the treatment was effective. I feel confident again." – Neha S.
"The procedure was quick, and the recovery was smooth. I'm grateful for the professional and empathetic approach." – Priya M.
Frequently Asked Questions
Are vulval warts dangerous?
While vulval warts are caused by HPV and are generally benign, they can cause discomfort and emotional distress. It's essential to consult a healthcare provider for appropriate evaluation and treatment.
Can vulval warts come back after treatment?
Yes, warts can recur, especially if the underlying HPV infection persists. Regular follow-ups and monitoring are recommended.
Is the removal procedure painful?
Most treatments are performed under local anesthesia, minimizing discomfort. Some post-procedure soreness or irritation may occur but is typically manageable.
How can I prevent vulval warts?
Practicing safe sex, limiting the number of sexual partners, and receiving the HPV vaccine can reduce the risk of developing vulval warts.
Is the treatment covered by insurance?
Coverage varies depending on the insurance provider and the specific treatment method. It's advisable to check with your insurance company beforehand.
Contact Dr. Rainee Agrawal
For consultations and appointments:
Contact Us+91 9179559565
Contact Person: Dr. Rainee Agrawal